West Syndrome (Infantile Spasm)
From EEGpedia
West syndrome
Background
- Severe epilepsy syndrome with the triad:
- Infantile spasm
- Hypsarrhythmia
- Mental retardation
- Onset: 90% in the first 12 months after birth, with a peak onset between 4 and 6 months
- Incedence: 3 to 5/10,000 live births
- 2% of childhood epilepsies
- Classified according to etiology (old International League Against Epilepsy (ILAE) classification)
- Symptomatic (almost any disorder than can cause brain damage) ie:
- Trisomy 21 (Down syndrome)
- Trauma
- Infectious (meningitis, encephalitis)
- Metabolic disorders (ie maple syrup urine disease, mitochondrial encephalopathy, pyridoxine dependency)
- Hydrocephalus/microcephaly
- Tuberous sclerosis
- Ischemic encephalopathy
- Cryptogenic
- If a symptomatic cause is most probable, however the cause is not identified.
- 8-42% of the West syndromes
- Idiopathic
- 9-14% of the West syndromes
- In contrast to cryptogenic West, there is a normal development until the onset.
- No MRI abnormalities
- Symptomatic (almost any disorder than can cause brain damage) ie:
- New International League Against Epilepsy (ILAE) classification:
- Genetic
- Structural/metabolic
- Unknown
Clinic
- Psychomotor arrest or regression
- Spasms, sudden contraction of the trunk en limb lasting around 2 - 10 seconds
- Flexor spasm (Salaam spasm): Rapid bending of the head and torso forward and simultaneous raising and bending of the arms, similar to the greeting between muslims (Salaam)
- Extensor spasm: Extension of the neck and trunk and with extension and abduction of the limbs
- Mixed spasm
- 1 to 30 clusters/day of 20 to 100 spasms each cluster
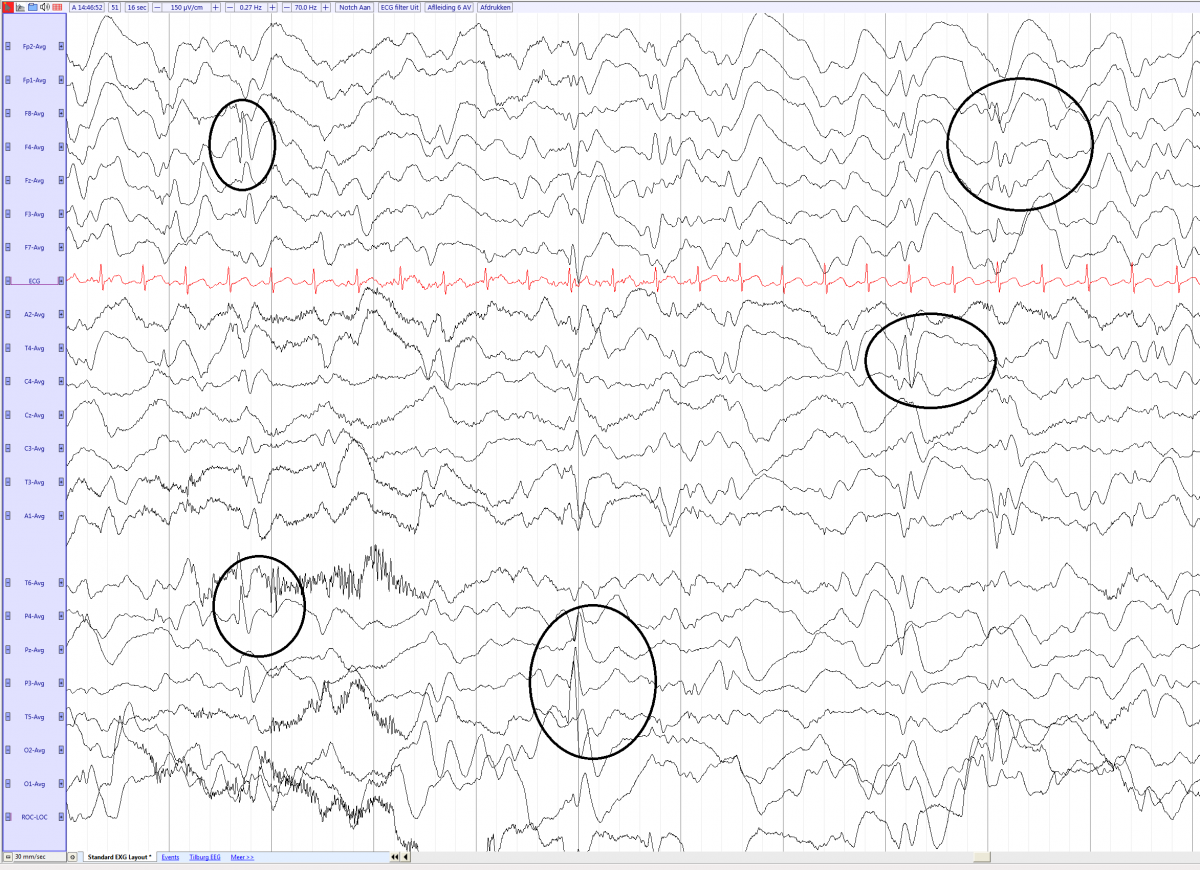
EEG
Interictal:
- Hypsarrhythmia: high voltage, chaotic, slow waves and spikes in all cortical areas. The spikes originate from multiple foci and have no rhythmical or repetitive organization.
- The typical hypsarrhythmia is usually seen in the early stage of West syndrome
- The EEG gradually evolves to a more synchronized, with increased hemispheric synchronization en symmetry.
- Hypsarrhytmia is most pronounced in sleep and the patients have reduces or absent non-REM sleep.
- Other interictal patterns: diffused (encephalopathic) or focal slowing, multifocal Spike slow wave complex
- The EEG can evolve towards a EEG seen in Lennox Gastaut Syndrome
Ictal EEG
- High-voltage, frontal dominant, generalized slow-wave transient followed by voltage attenuation
West syndrome with hypsarrhytmia (multifocal spike and slow waves, with little organization) in a 8 months old girl (average)