Lennox Gastaut Syndrome
From EEGpedia
Contents
Background
- Severe seizures in childhood
- Presentation before eight years of age, most commonly between three and five years of age
- Many cases evolve into Lennox Gastaut from other epilepsy syndromes, particularly West Syndrome (Infantile Spasm)
Clinics
- Mixture of seizure types
- Tonic
- Tonic-clonic
- Atonic (drop attacks)
- Myoclonic
- atypical absences
- Brief tonic seizures of seconds to 1 minute.
- The seizures can cause falls.
- Eyelid retraction, staring, mydriasis, and apnea are commonly associated
- The seizures are frequent
- Mental retardation before seizure onset in 20-60%
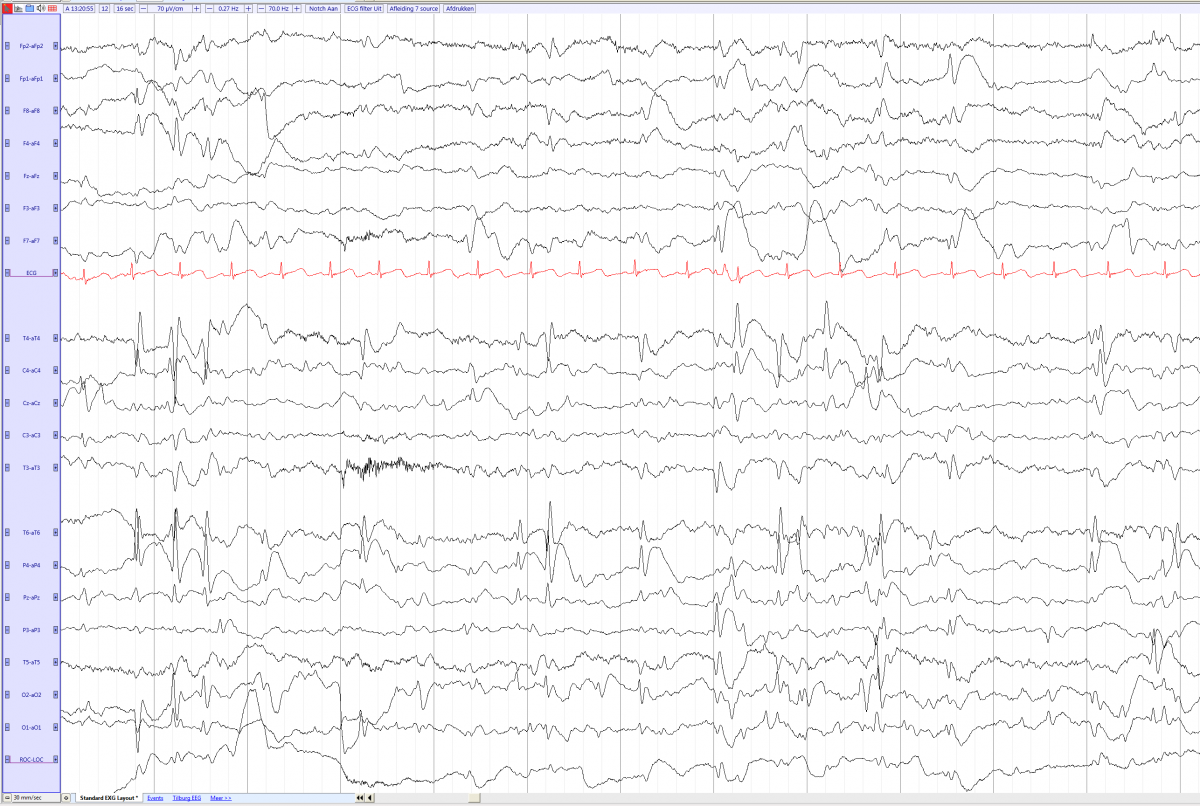
EEG
- Spike slow wave complex superimposed on an abnormal, slow background.
- The Spike slow wave complex and Sharp wave slow wave complex are generalized at a frequency of 1.5 to 2.5 Hz (slow), usually with the highest amplitude frontal.
- Transient and shifting asymmetries are frequent
- Non-REM sleep increases the discharges. In REM sleep the discharges decreases.
- Hyperventilation or photic stimulation does not trigger the discharges.
Ictal EEG
- Tonic seizure: typically fast rhythmic discarges of 10 – 20 Hz, increasing in amplitude.
- Myoclonic seizures: bursts of arrhythmic, multiple spike-wave or irregular spike-wave activity
- Atypical absence seizures: Slow (<2.5 Hz) and often asymmetric and irregular spike-and-wave activity
Treatment
- No drug is highly effective
- Valproic acid, lamotrigine, topiramate, rufinamide, felbamate, and clobazam can be effective
- Carbamazepine can worsen the drop attacks
Lennox gastaut in a 3 years and 10 months old boy (source) with multiple spike and slow waves and a slow basic rhythm